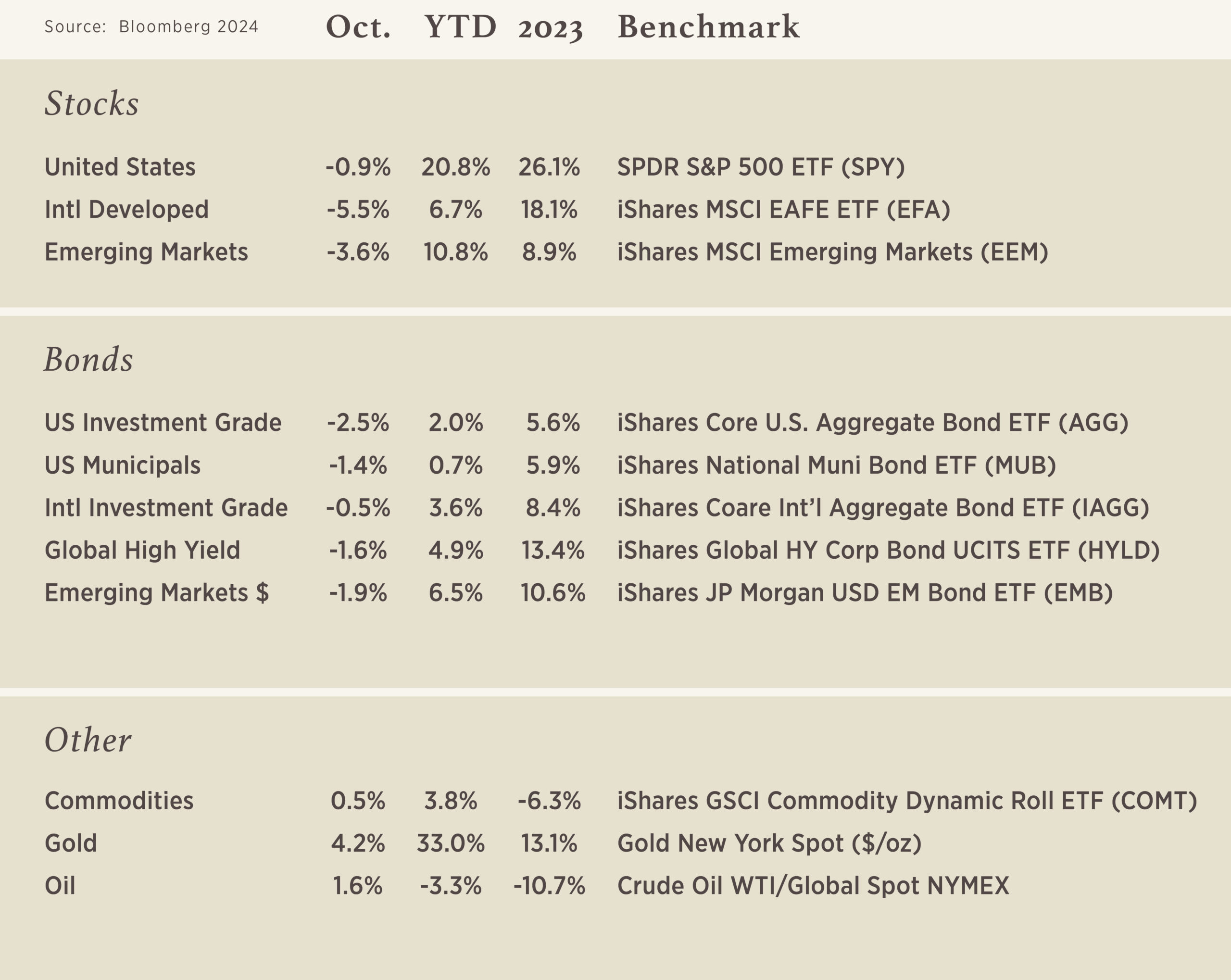
Chart of the Month

We often talk about the proverbial “crystal ball,” but would it really make much difference if we had it? Some evidence would suggest that it may not be as helpful as it may seem on the surface. The most recent example is articulated by oil prices – as shown in our chart – but prior instances, such as Trump’s win in 2016 and the onset of COVID, also highlight the difficulty of forecasting.
If we had told you that Russia would engage in war for 2.5 years (and ongoing) plus some of the Middle East powers would fight amongst each other for a year (and ongoing) – would the “crystal ball” have told us that oil is undoubtedly going to trade higher? Probably so! And it did for a while, but even as those two situations remain ongoing, oil prices now sit lower than they were prior to the initial event of Russia’s invasion of Ukraine in February 2022.
Immediately following the Russian invasion, oil jumped 34% over the following two weeks to hit its peak ($124/bbl). And in the two weeks following the attack on Israel, prices jumped 8%. However, oil prices today are 25% lower than the day before Russia’s invasion1, 44% lower than its peak2, and 16% lower since Israel was first attacked.3
Regarding Trump’s victory in 2016, you can find many anecdotes suggesting the equities would tumble, but the exact opposite occurred as equities rallied and never looked back. The same holds for COVID – sure equities plummeted initially – but the S&P 500 ended +18.5% between 2/15/2020 and 2/15/2021.4
All of this is to say that predicting the future is incredibly challenging, even if you knew what the headlines were going to read the next day. The optimal course is “staying the course.”
If you want to give your predictive abilities a try, a group called Elm Wealth has put together a brief game called Elm Crystal Ball Challenge, in which you can read “tomorrow’s headlines” and determine how you would position a portfolio as a result.
Source: Bloomberg
Dates:
1Day before Russia invaded Ukraine (2/23/2022)
2Peak oil price was 3/8/2022
3Day before Israel was attacked (10/6/2023)
4S&P Return

Eldercare ABCs: Unraveling Caregiving Terms
Helping an aging loved one will likely expose you to many new terms and some doctor-speak that will confound you at an already challenging time. Previewing some of these terms should make it easier for you to understand the decisions and choices that you have to make or take a role in deciding.
The AARP recommends that when you hear any phrase from a doctor, nurse or social worker that you don’t understand, speak up immediately to ask about it. If you don’t politely interrupt, you could forget what you wanted to ask by the end of the conversation.
Also, these appointments and consultations can be stressful, so it’s wise to take notes on what the medical professionals say and recommend.
Here are more than 75 terms that caregivers are likely to encounter:
Medical Terms and Specialties
- Acute care. Medical care given for a short time to treat a specific illness or condition. This can include doctor visits, short hospital stays or surgery.
- Alzheimer’s disease. A type of progressive mental deterioration, affecting memory and the ability to process thoughts, that is one form of dementia.
- Chronic disease. A condition that lasts one year or more and either requires ongoing medical attention or limits a person’s ability to bathe, care for themselves, dress, eat or walk.
- Comorbidity. The presence, or coexistence, of more than one disorder in the same person. They can occur at the same time or one after the other. Interactions between the illnesses can worsen the course of both.
- Continence. The ability to control bowel and bladder function.
- Delirium. Short-term confused thinking and disrupted attention usually accompanied by disordered speech and hallucinations.
- Dementia. A general term for a decline in mental ability severe enough to interfere with daily life. Memory loss is an example. Alzheimer’s disease is the most common cause of dementia, but not all dementia comes from Alzheimer’s.
- Vital signs. Signs of life — specifically, a person’s heart rate (pulse), breathing rate, body temperature and blood pressure. They show doctors how well a person’s body is functioning.
Legal Documents and Descriptions
- Advance directives. Written statements that communicate individuals’ medical preferences if they become unable to make their own health care decisions. The two types include a living will that spells out medical treatment the individual would want at the end of life if they can’t speak for themselves; and a health care proxy, which identifies a health care agent to serve as spokesperson on medical decisions for an individual who can’t communicate.
- Competence. In a legal sense, a person’s ability to understand information, make a choice based on that information and communicate that decision in an understandable way.
- Conservator. A person whom a court appoints to handle someone’s affairs when that person cannot do the job. Usually, a conservator handles only finances.
- Do not resuscitate (DNR) order. A type of advance directive in which a person states that health care providers should not attempt to restart the heart through cardiopulmonary resuscitation if the heart or breathing stops.
- Durable power of attorney. A legal document that gives someone you choose the authority to act financially, legally and medically in your place if you become incapacitated and unable to handle matters on your own. It remains in effect until the person who grants it either cancels it or dies.
- Family and Medical Leave Act (FMLA). A federal labor law that provides certain employees with up to 12 weeks per year of unpaid, job-protected leave to accommodate some family and medical situations. The law also requires that employees’ group health benefits be maintained during the leave.
- Guardianship. A court-sanctioned legal relationship in which a person is given legal authority over another when that other person is unable to make safe and sound decisions regarding his or her person or property.
- Health care proxy. A type of durable power of attorney in which people appoint another person to make health care decisions for them if they become unable to do so.
- Informed consent. The process of making decisions about medical care or medical experimentation based on open and honest communication among the health care provider, the patient and the patient’s family.
- Living will. A legal document in which the signer requests to be allowed to die rather than be kept alive by artificial means if disabled beyond a reasonable expectation of recovery.
- Power of attorney (POA). A legal document that gives someone you choose the authority to act on your behalf, usually on financial matters.
- Sundown syndrome or sundowning. A state of confusion that occurs later in the afternoon and into the night. It is most often found in patients who have dementia or Alzheimer’s disease and includes a range of behaviors such as increased confusion, anxiety, agitation and sleeplessness.
- Surrogate. An individual appointed to act in place of another.
Housing and Health Services
- Adult care home, adult family-care home (AFCH) or group home. A small, assisted living residence where employees provide for disabled adults or seniors who need help with certain tasks but want to remain as independent as possible. They are an alternative to more restrictive, institutional settings, such as nursing homes, which provide 24-hour nursing care.
- Adult day care. Centers that provide companionship and help to older adults who need supervision during the day. The programs can help give a break to a round-the-clock caregiver.
- Activities of daily living (ADLs). Actions a person must do by themselves to engage independently in everyday life, such as bathing, dressing, eating, being mobile, moving from bed to a chair, and using the toilet.
- Assisted living facility (ALF). Housing for those who may need help living independently but do not need skilled nursing care. The level of assistance varies among residences and may include help with bathing, dressing, meals and housekeeping.
- Cohousing. A small, planned community in which single-family homes, townhouses or rental units are clustered around amenities such as a community kitchen and dining room, common areas for sitting, craft and meeting rooms, gardens, and potentially adult and child day care. The goal is to design a neighborhood where people of all ages and family statuses can rely on the informal, mutual support of neighbors to help out.
- Consumer-directed personal assistance program. A Medicaid program available in several states that permits chronically ill and physically disabled people to choose, train and supervise workers who help them with activities of daily living such as bathing, light housework and meal preparation so they can remain in their homes. Some relatives and friends of participants can qualify to be paid through this program.
- Continuing care retirement community (CCRC). Housing that offers a variety of living options and services — including independent living, assisted living and skilled care, often all on the same campus — and is designed to meet a person’s changing needs.
- Custodial care. Nonmedical care that helps individuals with bathing, dressing and other basic care that most people do themselves, such as using eye drops. It can occur in a range of environments including adult day care, assisted living centers and residential care facilities.
- Extended care. Short-term or temporary care in a rehabilitation hospital or nursing home with the goal of returning a patient home.
- Independent living. An age-restricted option for a house, condominium or apartment — sometimes offered as part of a continuing care retirement community — that has few services as part of the basic rate. Those that are included are more often related to convenience, such as grass cutting or a clubhouse.
- Meals on Wheels. A service that delivers daily hot meals to the homes of elderly or disabled people.
- Memory care communities. Separate facilities or specialized units of an assisted living center that focus on helping people with Alzheimer’s disease and other forms of dementia, where the staff is specifically trained to deal with recall problems and other impairments.
- Nursing home. A public or private residential facility providing a high level of long-term personal or medical care for chronically ill, disabled and older people who are unable to care for themselves properly.
- Respite care. Short-term or temporary care of sick, disabled or older persons for a few hours, days or weeks, designed to provide relief to the regular caregiver.
- Rehabilitation hospital. A medical facility providing therapy and training for the restoration of physical function or cognitive skills following a serious injury, illness or medical event (such as a stroke).
- Senior center. A physical location providing opportunities for older adults to get active, enjoy various social activities and improve their overall quality of life.
- Skilled care. Nursing or rehabilitation services that a doctor orders and that licensed health professionals such as nurses and physical therapists provide.
Technology
- Assistive technology devices. Products that improve a person’s ability to live and function independently. Low-tech assistive devices include canes and pill organizers; high-tech items include electric wheelchairs, hearing aids and smartphones.
- Personal emergency response system (PERS), also known as a medical alert system. An alarm system that lets someone experiencing a medical or personal emergency such as a fall summon help. Traditional systems are triggered by the user pressing a button on a wearable device like a bracelet, sending a radio signal to a console connected to a phone, which calls an emergency response center. In recent years, some smartphones and other connected devices like smartwatches have incorporated medical alert functions.
- Remote patient monitoring (RPM). A subcategory of telehealth services that allows patients to use mobile medical devices and technology to gather patient-generated health data, such as weight, blood pressure and heart rate, and send it to health care professionals.
Insurance Terms
- Copayment, sometimes called copays. A fixed amount — $20, for example — that one pays for a health care service covered by insurance after payment of the deductible. Let’s say your health plan’s allowable cost for a doctor’s office visit is $100. If you haven’t yet met your deductible for the year, you’ll pay the full $100. If you have met the deductible, you pay the $20 copay, usually at the time of the visit.
- Long-term care insurance. Coverage that helps policyholders pay for long-term care in their home or at a nursing home or assisted living facility, or for other designated services, depending on the policy.
Specialist Roles and Responsibilities
- Cardiologist. A medical doctor who specializes in heart disorders.
- Dermatologist. A medical doctor who specializes in skin disorders.
- Discharge planner. A professional who assists patients and their families in developing a method of care for a patient following a hospital or nursing home stay.
- End-of-life doula, also known as a death doula. An individual who provides nonmedical comfort and support to a dying person and their family. This may include education and guidance as well as emotional, spiritual or practical care.
- Endocrinologist. A medical doctor who specializes in hormonal and metabolic disorders, including diabetes.
- Family or informal caregiver. Any relative, partner, friend or neighbor who has a significant personal relationship with and provides a broad range of assistance for an adult with a chronic or disabling condition.
- Gastroenterologist. A medical doctor who specializes in digestive orders.
- Geriatric care manager, also called an aging life care professional. A specialist who assesses a person’s mental, physical, environmental and financial conditions to create a care plan to assist in arranging housing, medical, social and other services.
- Geriatrician. A medical doctor who has completed a residency in either family medicine or internal medicine and focuses on older adults.
- Hematologist. A medical doctor who specializes in blood disorders.
- Home health agency. A company or nonprofit, often certified by Medicare, that provides health-related services such as nursing, personal care, social work, or occupational, physical or speech therapy in a client’s home.
- Home health aide (HHA). A trained and certified health care worker who assists a patient in the home. Duties typically include help with hygiene and exercise, light household work such as meal preparation, and monitoring the patient’s condition.
- Homemaker services. Light housekeeping, meal preparation, washing clothes, shopping and other tasks workers from state-certified agencies perform for people who need assistance in their homes. Medicare does not cover these services, but some states’ Medicaid programs help qualified low-income adults pay for them.
- Hospice care. A treatment regime for people who have an advanced, life-limiting, often incurable illnesses. Considered a type of palliative care, hospice focuses on the patient’s psychological well-being and on managing symptoms of a disease rather than the disease itself, so they can spend their last days with dignity and quality, surrounded by loved ones.
- Licensed practical nurse (LPN). A person who has completed nursing or vocational training and obtained a state license that authorizes the person to take care of basic duties in settings such as hospitals, nursing homes and long-term care facilities.
- Long-term care ombudsman. An advocate for residents of nursing homes, residential care homes and assisted living facilities. Ombudsmen are trained to resolve problems; they provide information on how to find a facility and what to do to get high-quality care.
- Nephrologist. A medical doctor who specializes in kidney disorders.
- Neurologist. A medical doctor who specializes in nervous system disorders.
- Nurse practitioner (NP), also known as advanced practice registered nurse (APRN). A primary-care provider with graduate training in advanced practice nursing who has the authority to order tests, write referrals and prescribe medicines.
- Patient advocate. A professional who can resolve concerns about someone’s health care experience, particularly problems that cannot be taken care of immediately.
- Personal care services (PCS). A broad term used to refer to help with personal hygiene and other self-care, such as bathing, dressing, eating, going to the bathroom, maintaining personal appearance and walking, provided by in-home personal care aides (PCAs). Some PCAs also help with meal preparation, grocery shopping and money management.
- Physician assistant (PA). A health care professional with a master’s degree who works in collaboration with a medical doctor or doctor of osteopathic medicine, often in a primary care setting.
- Podiatrist (DPM). A doctor with specialized training in treating foot and ankle problems.
- Primary care physician (PCP). The doctor that you see first for checkups and health problems. Sometimes these health care professionals have family practices for all ages; others specialize in internal medicine for adults or pediatrics for children.
- Psychiatrist. A medical doctor who specializes in emotional and mental disorders.
- Psychologist. A specialist, but not a medical doctor, who can talk with patients and their families about emotional and personal matters and can help them make decisions.
- Radiologist. A medical doctor who specializes in X-rays and related procedures such as computed tomography (CT) scans, magnetic resonance imaging (MRI) and ultrasound tests.
- Registered nurse (RN). A health professional who has graduated from a nursing program, passed a state board examination, and has a state license.
- Rheumatologist. A medical doctor who specializes in pain and other symptoms related to joints and other parts of the musculoskeletal system, such as bones, cartilage, ligaments, muscles and tendons.
- Urologist. A medical doctor who specializes in disorders of the male reproductive system as well as the male and female urinary tract.
Medicaid, Medicare & Social Security
- Medicaid. Government-provided health care coverage for eligible low-income adults, children, pregnant women, elderly adults and people with disabilities. States and the U.S. government share the cost of Medicaid, with states administering the program according to federal requirements. As of May 2021, nearly 76 million people were covered in Medicaid, and enrollment has grown by more than 18 percent during the COVID-19 pandemic.
- Medicare. A federal government program that provides medical insurance if you are 65 or older, under 65 and receiving Social Security Disability Insurance, or under 65 and diagnosed with end-stage renal disease (ESRD). Medicare Part A is hospital insurance, and Medicare Part B covers certain doctors’ services, outpatient care, medical supplies and preventive services. In 2020, 62.6 million people were enrolled in Medicare, 54.1 million of them on the basis of age.
- Medicare Advantage, also called Medicare Part C. Private health plans that offer all benefits covered by “original” Medicare (parts A and B) but may also provide non-Medicare-covered benefits such as prescription drug coverage, dental and vision coverage, and even gym memberships, usually for an additional premium.
- Medicare Savings Program (MSP). A federally funded, state-administered program that helps people with limited income and resources pay some or all of their Medicare premiums, deductibles, copayments and coinsurance. Four types of MSP are available:
1. Qualified Medicare Beneficiary (QMB) for people also enrolled in Medicaid
2. Specified Low-Income Medicare Beneficiary (SLMB), which helps pay for Part B premiums only
3. Qualifying Individual programs (QI and QI-1), which have slightly higher income limits but still help pay for Part B only
4. Qualified Disabled & Working Individuals (QDWI), which helps pay for Part A premiums
- Medicare telehealth services. Medicare-covered visits with health care professionals conducted via phone or video chat. Initially offered on a limited basis to people in rural areas, these services expanded considerably during the COVID-19 pandemic.
- Medigap, also called Medicare Supplemental Insurance. Private policies designed to pay costs not covered using original Medicare. For example, Medigap plans might cover your Medicare copayments, coinsurance and deductibles, or services original Medicare doesn’t cover, such as care when you travel outside the United States.
- Social Security. The U.S. government’s social insurance program, providing monthly benefit payments to retired workers age 62 and older; their spouses (or ex-spouses), children and survivors; and people with disabilities that prevent them from working for an extended period. The system is funded by payroll tax contributions workers make throughout their careers, with monthly benefit amounts determined primarily by their lifetime earnings history.
- Social Security Disability Insurance (SSDI). Monthly benefit payments to people below retirement age with a significant illness or impairment that prevents them from working for at least a year or is expected to result in death. Eligibility is based on past work in which the person paid Social Security taxes and is reviewed periodically to make sure the disability continues to restrict them from working.
- Supplemental Security Income (SSI). A program the Social Security Administration oversees that pays monthly benefits to people with limited income and resources who are disabled, blind, or age 65 or older.
Three levels of facility based-care
What is the level of care in a skilled nursing facility?
Skilled nursing care is provided by trained registered/licensed nurses in a medical setting under a doctor’s supervision. It’s basically the same level of nursing care you get in a hospital. Patients may go from the hospital to a skilled nursing facility to continue recovering after an illness, injury or surgery. In addition to skilled nursing, care may include rehabilitative services from licensed physical, occupational or speech therapists. A skilled nursing facility provides generally short-term transitional care. The goal is to get well enough to go home.
Skilled nursing facility care is funded by Medicare and commercial insurance for a limited period.
What is the level of care in a nursing home?
Nursing home care is provided mostly by licensed practical nurses and nurse aides under the supervision of a registered nurse. Care is focused on activities of daily living, like dressing, bathing and eating. This is often called “custodial care” or “long-term care.” People sometimes move to a nursing home when they are unable to take care of themselves due to medical, cognitive, behavioral or functional issues. In addition to custodial care, nursing home residents will get help taking medications and managing chronic conditions. A nursing home provides long-term residential care. The goal is to provide a safe, comfortable and caring environment for people who are unable to live independently.
Nursing home “custodial care” is not covered by Medicare or commercial insurance. Residents pay privately or may be covered by their long-term care insurance. Medicaid will cover this care when the person’s resources are exhausted, and almost every nursing home is a provider in the Medicaid program.
What level of care is assisted living?
Assisted living is a residence for older people or people with disabilities who require help with some of the activities and routines of daily living as well as access to medical care when needed. In terms of the level of care provided, assisted living is a step below a nursing home or skilled nursing facility care.
Assisted living care is not covered by Medicare or commercial insurance. Residents pay privately or may be covered by their long-term care insurance. When their funds are depleted, most facilities require the resident to move to a nursing home because very few assisted living facilities participate as providers in the Medicaid program.
Source: AARP’s Caregiver Glossary.
Source: National Institutes of Health’ National Institute on Aging.